Immune cells may facilitate tumor growth by forming primitive vascular channels
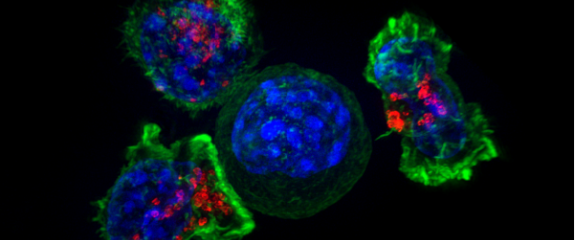
A new study led by scientists to suggest that there may be a way to limit tumour growth by targeting macrophages. Macrophages can 'drill' through tumors to create new vessel-like structures for oxygen and nutrient delivery as tumours grow. It may serve as a new therapeutic target for treating tumours.
A Different Kind of Vessel
In cancer, tumour cells stimulate angiogenesis whereby endothelial cells are induced to build new vessels. However, research reveals that not all vessels are lined by endothelial cells. In cancer, vessel-like structures can be created by a non-endothelial cell type. Called 'vascular mimicry', it occurs in various solid tumours like glioblastoma, breast cancer and melanoma. Occurrence has been attributed to a sub-population of cells within the tumour termed cancer stem cells.
In the presnt study found that macrophages can form vascular mimicry channels in tumours, as well as in other low-oxygen environments. Although macrophages are key cells of the immune system that recognize and attack foreign invaders and cancer cells, macrophages can be re-programmed within the tumour environment to promote tumour growth. The authors proposed a new and previously unrecognized structural role for macrophages in the formation of a vascular mimicry network connected to the systemic circulation. They used intravenously injected dye to delineate the established vasculature as well as the newly formed vascular mimicry conduits The researchers found that macrophages quickly migrate to oxygen-deprived environments and form these vessel-like channels. The tubular structures are lined with cells that express macrophage cell surface markers. The vessel-like channels appeared too small to carry red blood cells, but the researchers believe that the low oxygen concentrations within tumours drive macrophages to form this network of channels to transport dissolved oxygen and glucose.
The findings could explain why current drugs to slow angiogenesis do not slow tumour growth in some patients. The authors propose that future cancer therapies could starve tumours by combining current vessel-targeting drugs with drugs to influence macrophage activity. They propose that future studies could focus on better understanding how macrophages influence retinal angiogenesis and blood flow in the eye—a key concern for people with diseases like age-related wet macular degeneration, where leaky vessels can cause vision loss.